When someone with diabetes experiences dangerously low blood sugar and can’t eat or drink, a glucagon emergency kit becomes a life-saving tool that can prevent unconsciousness, seizures, or worse outcomes.
Many people feel overwhelmed by the idea of giving an emergency injection, but glucagon kits are designed for non-medical caregivers to use during critical situations. It’s important to act quickly because severe low blood sugar can cause brain damage or death if left untreated.
Understanding how to properly prepare and administer glucagon can mean the difference between a medical emergency and a manageable situation. Our step-by-step approach will help us feel prepared and confident when every second counts.
Key Takeaways
- Mix the glucagon powder with sterile water before injecting it into muscle tissue during severe low blood sugar emergencies
- Call emergency services immediately after giving glucagon and turn the unconscious person on their side to prevent choking
- Practice using the kit beforehand and ensure family members know where we keep it and how to use it properly
Table of Contents
Step-by-Step Instructions for Using a Glucagon Emergency Kit
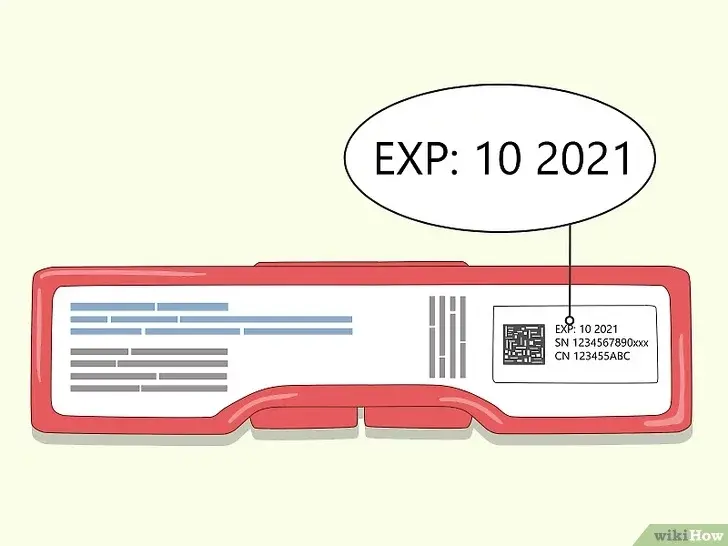
1. Check expiration date — replace if expired.
Before using glucagon, make sure the kit is in date. Expired medication may not work effectively, and in an emergency, you can’t risk reduced potency. Always keep a fresh kit ready.
2. Remove the vial cap and needle cover.
Take off the plastic cap from the vial of glucagon powder and the protective cover from the syringe needle. This prepares the components for mixing without delay.
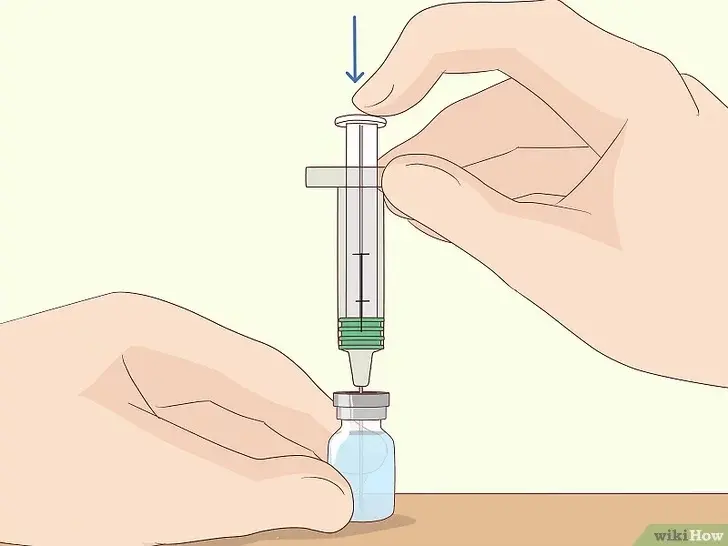
3. Inject all sterile water from the syringe into the glucagon vial.
Push the syringe plunger fully so the sterile water flows into the vial. This is necessary to dissolve the powdered glucagon before it can be used.

4. Gently swirl until powder dissolves completely (solution should be clear).
Tilt and rotate the vial slowly rather than shaking hard. The liquid should become completely clear — if it looks cloudy or has particles, keep shaking. If it does not disolve properly, do not use it.

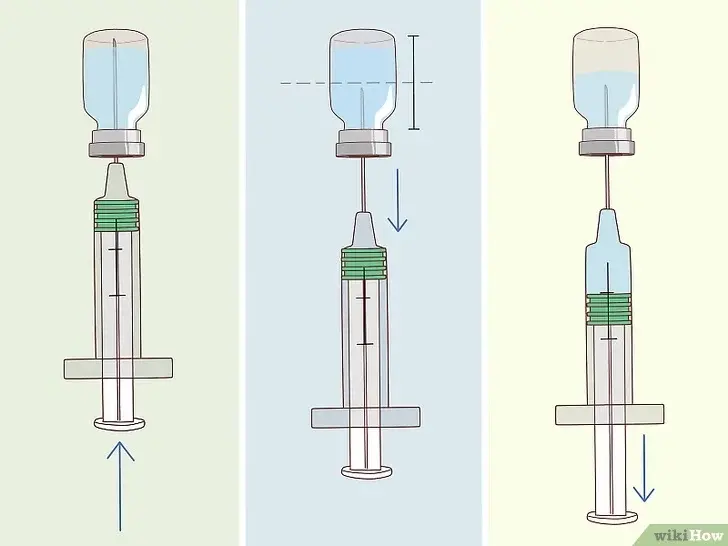
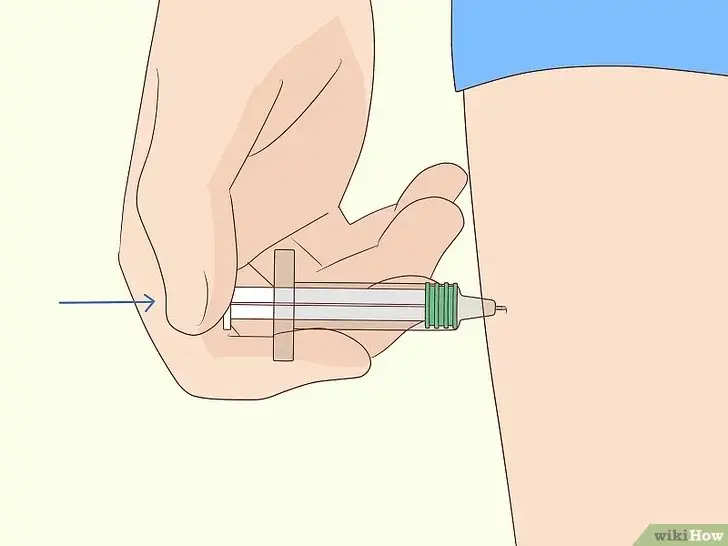
5. Draw all liquid back into the syringe, removing any air bubbles.
Turn the vial upside down and pull back the plunger to collect the full dose. Tap the syringe gently to move bubbles to the top, then push them back into the vial.
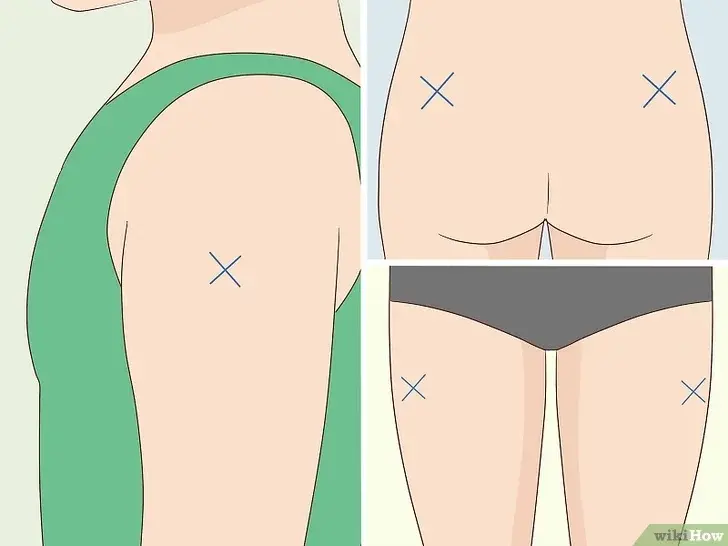
6. Choose an injection site — upper arm, thigh, or buttock.
Pick a location that’s easy to access quickly. These muscle areas allow glucagon to work faster during an emergency.
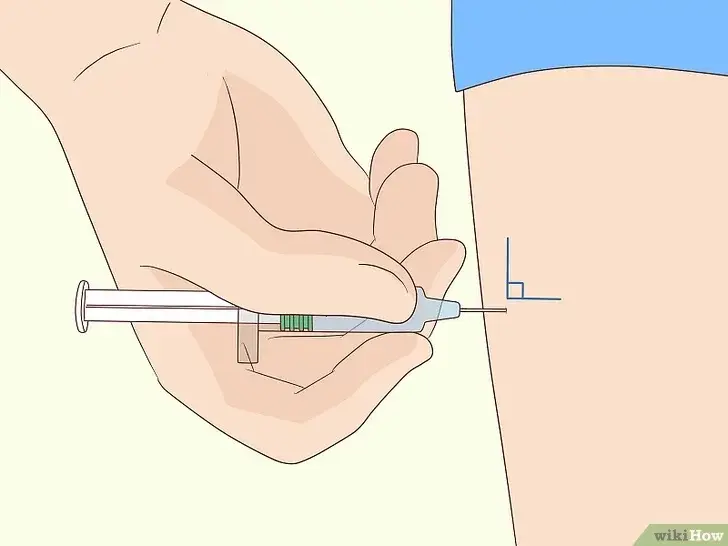
7. Insert the needle straight in, and push the plunger until empty.
Insert the needle straight in one smooth motion. Press the plunger fully to deliver the entire dose. Don’t hesitate when you feel a bit of resistance. The dosage needs to be administered to the person as fast as possible.
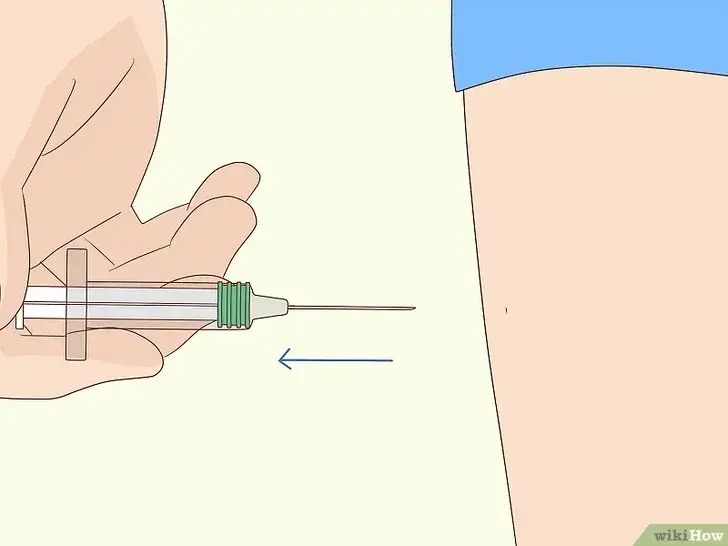
8. Remove the needle and apply gentle pressure to the site.
Pull the needle out quickly and press a cotton ball or gauze on the spot. This helps stop any bleeding and reduces soreness. Make sure to dispose the needle into a sharps container after use.

9. Turn the person on their side to prevent choking if they vomit.
As the medication starts working, nausea or vomiting can occur. Lying on their side keeps the airway clear and reduces the risk of choking.

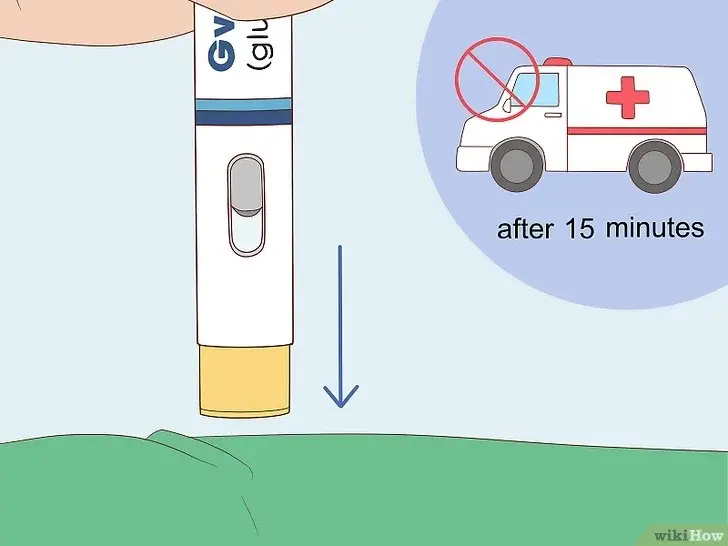
10. Call emergency services immediately, even if they wake up.
Severe low blood sugar is a medical emergency. Professional care is still needed to monitor recovery and prevent another episode. In the United States you can call 911. In Europe, the number 112 can be used.

Aftercare: What to Do After Giving Glucagon
Most people begin to recover within about 15 minutes after receiving glucagon. Stay close and watch for signs of improvement.
As soon as the person is fully awake and able to swallow safely, give them a fast-acting sugar such as fruit juice, regular (non-diet) soda, or glucose tablets. This helps raise their blood sugar quickly and stabilizes them in the short term.
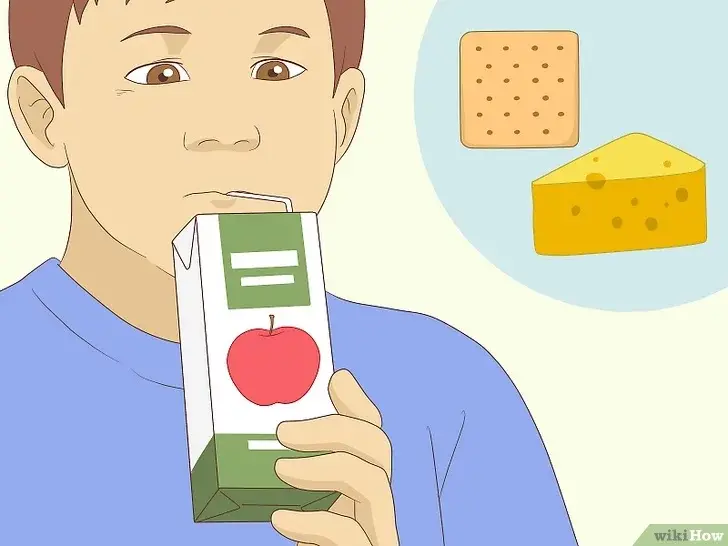
After the initial sugar, follow up with a long-acting carbohydrate like crackers with cheese, a peanut butter sandwich, or another snack that contains both carbs and protein. This will help maintain blood sugar levels and prevent another sudden drop.
Continue to monitor closely for recurring symptoms such as sweating, dizziness, or confusion. If the person does not show signs of improvement within 15 minutes, give a second glucagon dose if another kit is available, and continue waiting with them until emergency services arrive.
Understanding Glucagon Emergency Kits
Glucagon emergency kits contain life-saving medication that treats severe low blood sugar in people with diabetes.
What Is a Glucagon Emergency Kit?
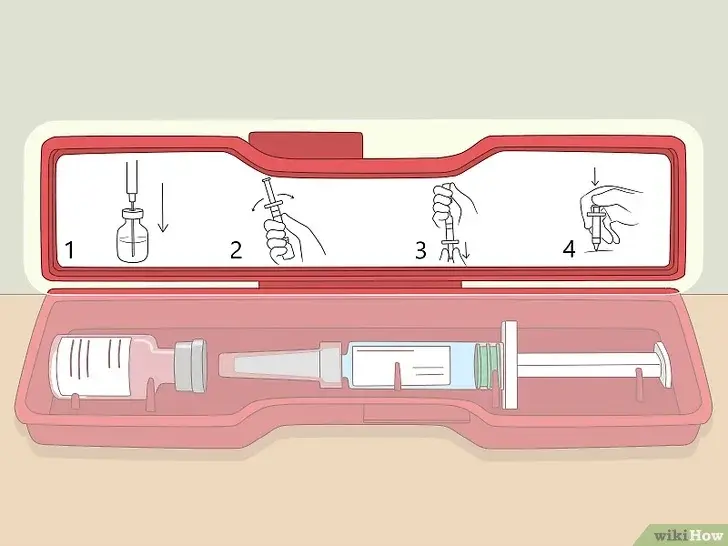
A glucagon emergency kit is a prescription medication designed to treat severe hypoglycemia when someone cannot eat or drink sugar. The kit contains three main components that work together to deliver this critical treatment.
Components:
- 1 vial with 1 mg of powdered glucagon
- 1 prefilled syringe with 1 mL sterile water
- 1 attached needle for injection
The glucagon comes as a dry powder that we must mix with the sterile water before use. This mixing step is essential because glucagon loses its strength quickly once prepared.
You cannot use any other liquid to mix the medication. The kit includes everything needed for one emergency dose.
The medication works by telling our liver to release stored sugar into the bloodstream. This raises blood sugar levels within 15 minutes of injection.
When to Use a Glucagon Emergency Kit
Use a glucagon emergency kit only when the person has severe hypoglycemia and cannot safely take sugar by mouth. If they’re conscious and able to swallow, offer a sugary snack or drink first before turning to a glucagon injection.
Emergency signs include:
- Unconsciousness
- Seizures
- Severe confusion or inability to follow instructions
- Inability to swallow without choking
⚠ Do NOT give food or drink to someone who is unconscious — this can cause choking. Instead, use glucagon and call emergency services immediately.
Glucagon Types and Formulations
The most common glucagon emergency kit contains 1 mg of glucagon for injection that requires mixing before use. This traditional formulation has been the standard treatment for decades.
Available Glucagon Forms:
- Powder form: Requires mixing with sterile water
- Pre-mixed auto-injectors: Ready to use without mixing
- Nasal spray (Baqsimi): No injection needed
Store all glucagon types at room temperature between 68°F to 77°F. Make sure to check expiration dates regularly and replace expired kits.
Most insurance plans cover glucagon emergency kits with a prescription. Keep kits in multiple locations like home, work, and school for quick access during emergencies.
Recognizing Severe Hypoglycemia
Severe hypoglycemia presents distinct warning signs that require immediate emergency treatment. Understanding when oral treatments are no longer effective helps us determine the right time to use glucagon.
Symptoms of Severe Low Blood Sugar
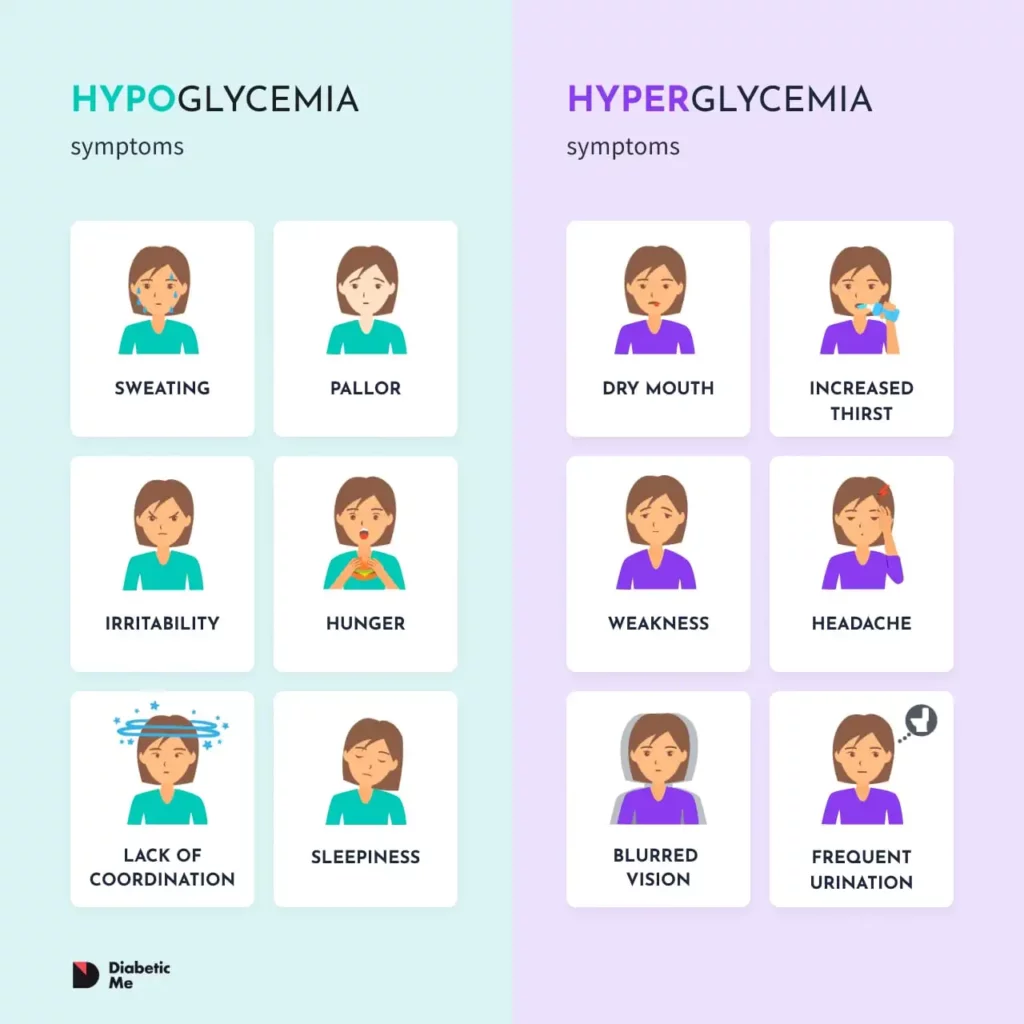
The most critical symptoms of severe low blood sugar include loss of consciousness and inability to swallow safely. These signs indicate we need emergency glucagon treatment.
Early warning signs you watch for include:
- Confusion and disorientation
- Slurred speech or difficulty speaking
- Seizures or convulsions
- Extreme drowsiness or unresponsiveness
Physical symptoms often appear alongside mental changes. Profuse sweating, rapid heartbeat, and trembling may occur before consciousness is lost.
The person may become aggressive during severe episodes. This behavior results from the brain not getting enough glucose to function normally.
Complete unconsciousness represents the most dangerous stage. At this point, the person cannot treat themselves with oral glucose tablets or juice.
Possible Side Effects and Reactions
Common side effects include nausea and vomiting when the person wakes up. This happens because glucagon affects the stomach.
Injection site reactions are frequent:
- Swelling
- Redness
- Pain or tenderness
Other common effects include:
- Nausea and vomiting
- Headache
- Dizziness
- Weakness
- Low blood pressure
- Pale skin
Serious allergic reactions can happen but are rare. Call for emergency help if someone develops difficulty breathing, severe rash, or very low blood pressure.
Prevention, Training, and Emergency Preparedness
Proper training and preparation can make the difference between a manageable emergency and a dangerous situation. Focus on educating those around us, maintaining our supplies properly, and taking steps to reduce hypoglycemia risks.
Educating Family, Friends, and Caregivers
Train multiple people in your live to use a glucagon emergency kit before an emergency happens. Family members and others should know where we keep our kit and how to use it properly.
Key people to train include:
- Spouse or partner
- Adult children or parents
- Close friends
- Coworkers
- Exercise partners
- Babysitters or caregivers
Practice the injection steps with your support network regularly. Show them how to mix the powder and liquid, where to inject, and what to expect after giving the shot.
Storing and Maintaining Your Glucagon Emergency Kit
Proper storage keeps our glucagon emergency kit ready when we need it most. Store glucagon at room temperature between 68° to 77°F (20° to 25°C) and never freeze it.
Storage requirements:
- Keep in original packaging
- Store away from light
- Maintain room temperature
- Check expiration dates regularly
- Replace expired kits immediately
Conclusion
Glucagon can save a life during severe hypoglycemia — but only if you and those around you know how to use it. Keep your kit accessible, practice the steps, and act fast when every second counts.
Frequently Asked Questions
What is the step-by-step process for administering a glucagon injection?
First, we check the expiration date on the kit. Remove the plastic cap from the bottle of glucagon powder.
Next, take the syringe and inject all the liquid into the bottle with the powder. Gently swirl the bottle to mix the contents until the solution becomes clear.
Draw the mixed glucagon back into the syringe, and choose an injection site on the arm, thigh, or buttocks.
Insert the needle at a 90-degree angle and inject all the medication. After injection, turn the person on their side to prevent choking if they vomit.
When should a glucagon emergency kit be used?
Use glucagon injection for severe hypoglycemia when people cannot take sugar by mouth. This happens when someone is unconscious, having seizures, or unable to safely swallow.
Blood sugar readings below 50 mg/dl signal the potential need for emergency glucagon. Also use it when someone shows confusion, coordination problems, or becomes uncooperative due to low blood sugar.
Severe low blood sugar is always an emergency that requires immediate action.
Are there any side effects to be aware of when using a glucagon kit?
Nausea and vomiting are the most common side effects after glucagon injection. This is why you turn the person on their side after giving the shot.
Some people may experience temporary increases in heart rate and blood pressure. Headaches can also occur as blood sugar levels rise.
These side effects are usually mild and temporary. The benefits of treating severe low blood sugar far outweigh these risks.
How should a glucagon emergency kit be stored?
Store glucagon kits at room temperature between 68-77°F. Keep them away from direct sunlight and heat sources.
The kit should not be frozen or refrigerated. Check expiration dates regularly and replace expired kits immediately.
