Preparing questions for your endocrinologist ensures you get the best care and leave your appointment with clear next steps. Endocrinologists help people with diabetes fine-tune treatment, review labs, adjust medications, and discuss lifestyle strategies. Asking the right questions improves blood sugar control and helps you stay proactive between visits.
Key Takeaways
- Visit your endocrinologist at least annually (often after quarterly labs).
- Bring blood sugar logs, medication lists, and test results for context.
- Ask about A1C targets, lab results, and whether medication or insulin adjustments are needed.
- Discuss self-management strategies for illness, exercise, and travel.
- Explore new treatments (CGMs, insulin pumps, GLP-1s, SGLT2 inhibitors).
- Address affordability of medications and get nutrition/exercise guidance.
Table of Contents
Getting Ready Before Your Visit
Think of your endocrinologist appointment like an important work meeting. This approach helps you stay organized and focused.
What to Bring:
- Pen and paper
- Written list of your main health concerns
- Questions you want to ask
- Blood sugar data from your devices
Write down your biggest worries before you go. This keeps you from forgetting important topics during your visit. Your doctor needs to understand what matters most to you.
If you use a continuous glucose monitor or blood sugar meter, bring that data to your appointment. Many phone apps can send this information directly to your doctor’s office ahead of time. Sharing your blood sugar data helps your endocrinologist tailor your diabetes management and treatment plan more effectively.
Quick Checklist:
- List of symptoms
- Current medications
- Blood sugar logs
- Insurance cards
- Previous test results
This preparation helps your doctor give you better care during your visit.
Medical History and Records
Bringing accurate and up-to-date medical records to your endocrinologist appointment is essential for effective hormone health management. Keep a detailed record of your medical conditions, current medications, lab work, and test results, including any relevant blood tests.
Don’t hesitate to request blood tests or ask about detecting diabetes-related antibodies if you have concerns. This information allows your endocrinologist to create a personalized treatment plan and ensures you receive the right care for your health needs.
Essential Questions for Your Endocrinologist Visit
Are My Current Diabetes Numbers Meeting My Personal Health Targets?
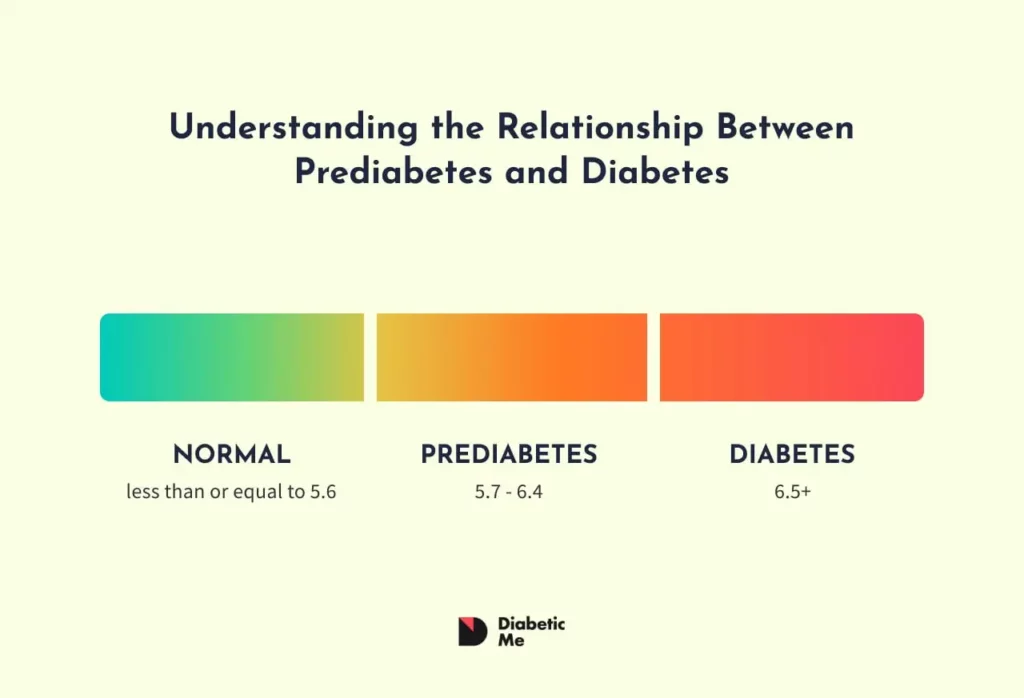
Understanding where you stand with your diabetes management helps you make better health choices. Your doctor typically orders lab tests before your appointment, including the A1C test that shows your average blood sugar levels over three months.
Ask your endocrinologist directly about your progress toward your specific goals. Your targets might change based on your life situation. If you’re planning to have a baby, you may need tighter control. If you experience frequent low blood sugar episodes, your doctor might suggest slightly higher targets.
| Life Stage | Typical A1C Goals |
|---|---|
| General adults | Under 7% |
| Pregnancy planning | Under 6.5% |
| Frequent lows | 7-8% |
| Older adults | 7.5-8.5% |
Make sure your diabetes goals match your current life phase and health needs.
Are My Other Lab Results Within Healthy Ranges?
Complete blood work checks more than just your A1C levels. These tests examine thyroid function, kidney health through urine protein, vitamin status, cholesterol numbers, blood cell counts, and more.
Talk with your doctor about any results that fall outside normal ranges. Pay special attention to markers for conditions common in people with diabetes:
- Hashimoto’s disease markers (Antithyroglobulin antibody)
- Celiac disease indicators (Tissue Transglutaminase Antibodies)
- Thyroid hormone levels that affect metabolism
Both Hashimoto’s and celiac disease happen more often in people with type 1 diabetes. These conditions can create hormone imbalances that make blood sugar control harder.
Do I Need Changes to My Diabetes Medications or Insulin Doses?
If you notice patterns of high or low blood sugar readings, meal-time spikes, or exercise-related sugar swings, discuss medication adjustments with your endocrinologist.
Your doctor can help you fine-tune several aspects of your treatment:
- Correction factors for high blood sugar
- Insulin sensitivity ratios
- Carbohydrate-to-insulin ratios
- Basal insulin rates throughout the day
Recent lifestyle changes often require medication adjustments. New exercise routines, stress, diet changes, pregnancy, or pregnancy planning can all affect your insulin needs and blood sugar targets.
What Can I Do to Manage My Care Between Office Visits?
You live with diabetes every day, but you see your doctor only a few times per year. Learning when and how to make your own adjustments helps you handle unexpected situations.
Ask your endocrinologist about self-management guidelines for different scenarios:
- Illness management: How much extra insulin to take when sick
- Exercise adjustments: Reducing insulin for increased physical activity
- Travel considerations: Managing time zone changes and schedule disruptions
Find out how to reach your medical team between visits. Some offices offer phone consultations, patient portals, or emergency contact options. Knowing these resources helps you get timely guidance when needed.
What Newer Treatment Options Should I Consider?
Diabetes treatments continue to improve rapidly. Newer insulins work faster and more predictably than older versions. Advanced technologies, like CGMs and insulin pumps, can automate much of your daily management.
Ask your doctor about:
- Newer insulin types that might work better for your lifestyle
- Continuous glucose monitors for real-time blood sugar tracking
- Insulin pump systems with automated delivery features
- Clinical trials for cutting-edge treatments
Should I Add Other Medications Beyond Insulin?
Sometimes insulin alone doesn’t provide optimal diabetes control. Your endocrinologist might suggest additional medications to address specific challenges.
Common supplemental medications for people with diabetes include:
- Metformin to improve insulin sensitivity
- GLP-1 agonists to reduce appetite and slow digestion
- SGLT2 inhibitors to help with weight management
- Pramlintide to control post-meal blood sugar spikes
These medications work differently than insulin and can address hormone imbalance issues that contribute to blood sugar problems. Each has specific benefits for different aspects of diabetes management.
How Can I Better Afford My Diabetes Medications?
Medication costs create real hardships for many people with diabetes. One in four Americans with diabetes report rationing insulin due to cost concerns.
Your endocrinologist can help you explore cost-reduction options:
Insurance Programs:
- Medicaid eligibility in your state
- Subsidized health plans through state exchanges
- Employer insurance optimization
Assistance Programs:
- Manufacturer discount programs
- Patient assistance foundations
- Federally Qualified Health Centers with reduced pricing
Don’t struggle alone with medication costs. Questions about affording diabetes care are common, and your doctor has resources to help.
How Should I Optimize My Eating Plan for Better Blood Sugar Control?
Diet plays a central role in diabetes management. Regular nutrition discussions with your endocrinologist help you identify foods that support or hinder your blood sugar control.
Review your typical meal patterns and discuss any foods causing consistent blood sugar spikes. Your doctor might suggest:
- Carbohydrate timing adjustments throughout the day
- Protein additions to slow sugar absorption
- Food substitutions for problem items
- Portion control strategies
Young people with diabetes face twice the risk of developing eating disorders compared to those without diabetes. Your endocrinologist can provide referrals to registered dietitians who specialize in diabetes nutrition if needed.
What Exercise Strategies Work Best for My Diabetes Management?
Physical activity improves insulin sensitivity and overall health, but it can also create blood sugar management challenges. Your endocrinologist can help you develop exercise strategies that work with your diabetes rather than against it.
Discuss specific exercise concerns:
- Pre-exercise insulin and food adjustments
- During-exercise blood sugar monitoring
- Post-exercise blood sugar patterns
- Activity timing relative to meals and insulin doses
Work with your doctor to create a plan that fits your fitness level and schedule while emphasizing the importance of maintaining physical function to support balance, mobility, and reduce the risk of complications.

hey Ely Fornoville, so I got to ask about that meds beyond insulin part, do you think theres stuff out there that’s actually gonna help me more than insulin does cuz im really not sure what to do here, any advice helps, thanks
Sam T, I’ve read that some meds can really change the game for you. might wanna keep an eye on the newer stuff, it’s all pretty interesting!
yeah but don’t forget insulin has been around for a long time for a reason. always talk to your doc before jumping onto anything new just cause you read about it online.